Femoral treatment with FlexiCones
Tip 1
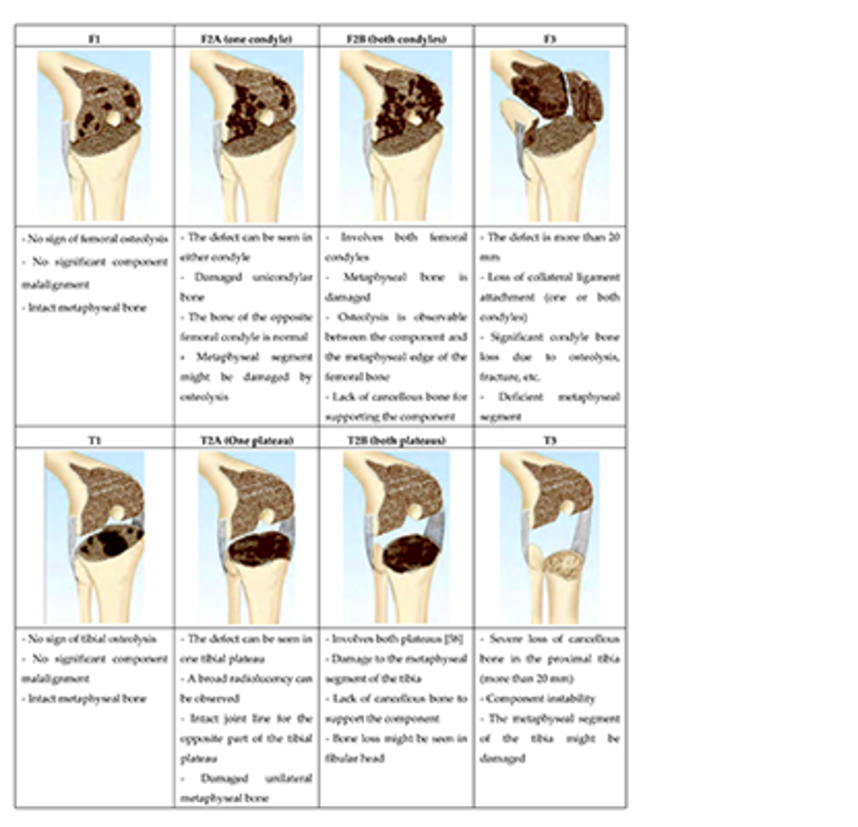
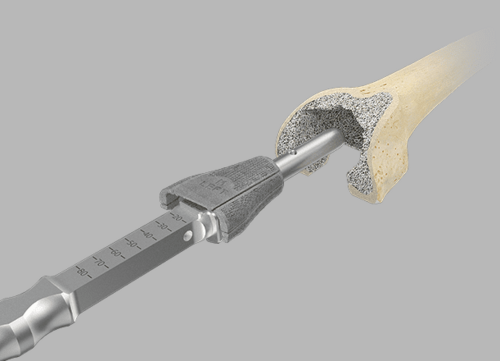
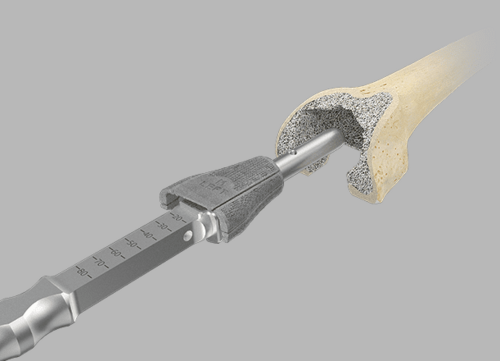
The zero position on the scale marked on the impactor indicates the level of the Femoral Cone/intracondylar box of Endo-Model femoral components.
Tip 2
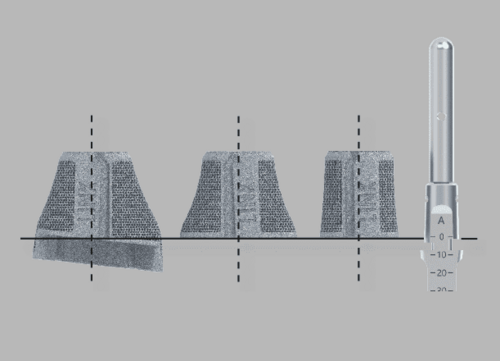
- Safety:
- Adapters can only be assembled in one direction in relation to the femoral impactor
- An integrated magnet in the femoral impactor helps in attaching the adapter in the correct position
- One-hand technique: The button on the rear of the impactor must be depressed and held down to attach the femoral compressor or final implant with the other free hand
Tip 3
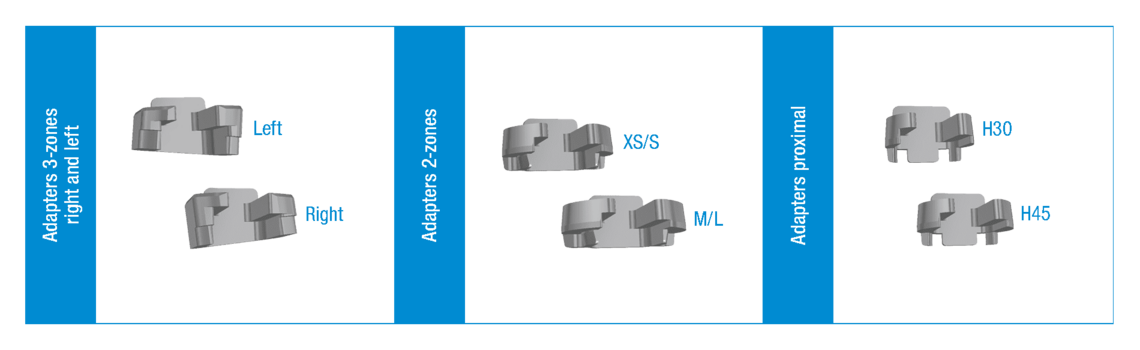
Double-check the correct choice of adapter, especially when using 2-zone or 3-zone cones. The laser marking is as follows (left/right or XS/S or H30/ H45)
Tip 4
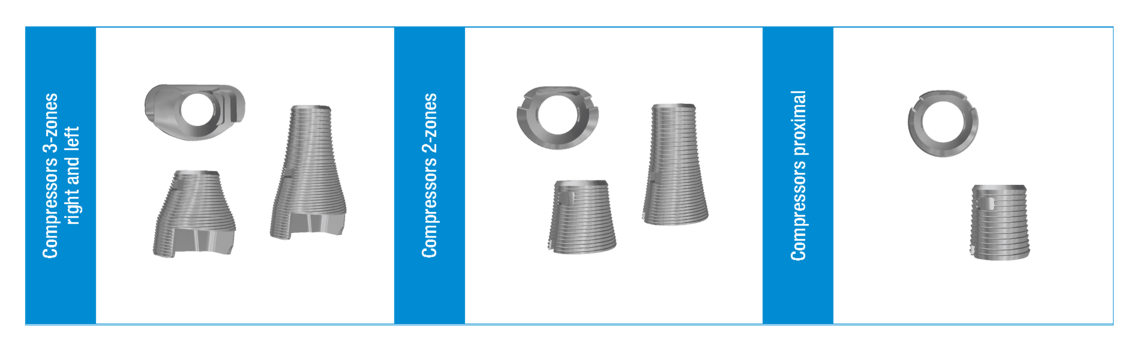
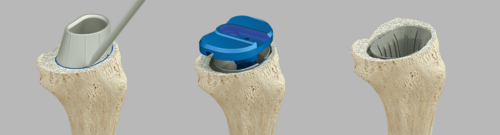
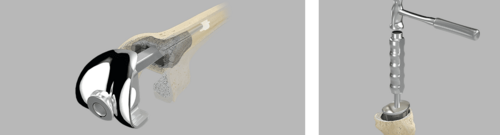
The Femoral Compressors have 2 functions. They serve as a rasp and as a trial implant. In order to check that the fit is correct, it is necessary to carry out a trial reduction with all the trial components from the Endo-Model Knee Family. After trial reduction, it may be advantageous to leave the femoral compressor in situ until shortly before implantation of the final implant.
Tip 5
Filling outer spaces Once the Femoral Cone has been placed, any spaces at the implant/bone interface can be filled with autologous material in order to achieve additional stability and prevent undesirable flow of cement between implant and bone.
Please note: Another option is to fill any outer spaces with bone graft material and compress
Tip 6
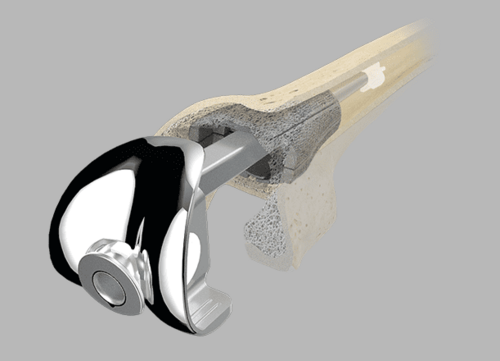
After implantation of the final Femoral Cone implant, it is recommended to double-check that it is correctly seated before placing the bone cement to fill the inner cavity.
This can be done with either the fully assembled femoral component (in the case of modular implant systems) or the femoral trial component. The purpose of the repeat trial, especially when using the 3-zone Femoral Cones, is to provide an intraoperative check for the appropriate box level between Femoral Cone and femoral knee component.
Tip 7
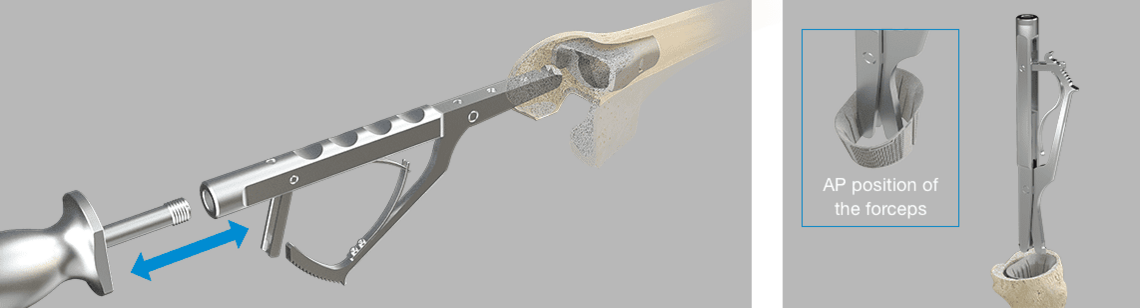
If it is necessary to reposition or explant the Femoral or Tibial Cone, the respective extraction forceps can be used after releasing the bony connection and removing the bone cement. In the event of a revision, both extraction forceps, i.e. for Femoral Cones or Tibial Cones, can be connected to the M12 thread of the forceps with a slap hammer.
After intramedullary insertion, the forceps grab underneath the cone rim. Repositioning of a Femoral Cone can also be done with the femoral impactor (see Tip 2).
Tip 8
Tibial Cones provide the same approach via the tibial trial cone.A reversed trial cone can be used to determine the version and size of Tibial Cone that needs to be inserted.
Another option is to fill and compress any outer spaces with bone graft material after placing the trial cone in trial positioning or repeat trial situations. After implantation of the final implant, it can again be advantageous to double-check that it is correctly seated before placing the bone cement to fill the inner cavity.
Tip 9
To prevent metal contact, it is recommended to make sure that the implant finishes somewhat distally below or proximally above (approx. 1 mm) the resection level.
Tip 10
When the Femoral Cone is implanted, its final seating should be approx. 1-2 mm ventral to the planned position of the intramedullary box.
TrabecuLink Cones: Biomechanical Analysis of TrabecuLink Flexible Femoral Cones in Endo-Model Hinged Total Knee Arthroplasty
Prof. Bernardo Innocenti, PhD
Major Findings
- Flexible Cone reduces bone stress during implantation, lowering the risk of bone fracture;
- Flexible Cone better distributes stress over the bone, improving implant stability;
- Flexible Cone does not alter the implant performance obtained with the rigid cones;
- Flexible Cone guarantees the same negligible implant micromotions obtained with the use of rigid cones.
To receive the complete FEA paper in print or PDF version, please contact us at info-flexicones@linkhh.de
Comparative Biomechanical In Vitro Study of Different Modular Total Knee Arthroplasty Revision Stems With Bone Defects
Dario Guttowski, Dr Med a, *, Valerie Polster, Dipl -Ing b, Gerd Huber, Dr Ing b, MichaelM.Morlock,Prof Dr b, Klaus Püschel, Prof Dr Med c, Jakob Nüchtern, PD,DrMed a
Abstract
Background
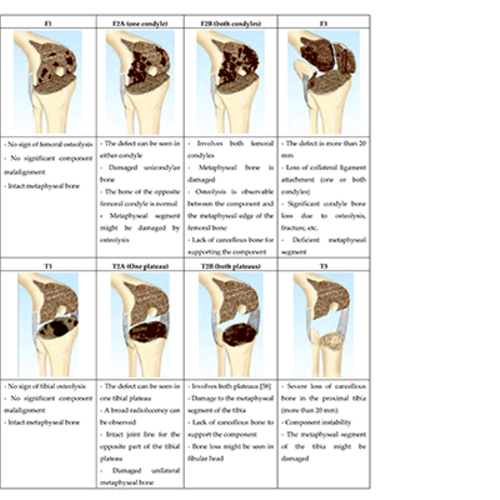
The aim of this study is to investigate the effects of different stem lengths and types including cones on primary stability in revision total knee arthroplasty with different femoral bone defects and fixation methods in order to maximize bone preservation. It is hypothesized that longer stems provide little additional mechanical stability.
Methods
Thirty-five human femurs were investigated. A distal bone defect, Anderson Orthopedic Research Institute classification (s. 33) type-F2a, was created in group 1-3 and type-F3 in group 4-6. A cemented, rotating hinge femoral component was combined with different stems (100 and 160 mm total or hybrid cemented cones, or a 100-mm custom-made anatomical cone stem). The femora were loaded according to in vivo loading during gait. Relative movements were measured to investigate primary stability. Pull-out testing was used to obtain a parameter for the primary stability of the construct.
Results
Relative movements were small and similar in all groups (<40 μm). For small defect, the pull-out forces of cemented long (4583 N) and short stems (4650 N) were similar and about twice as high as those of uncemented stems (2221 N). For large defects, short cemented stems with cones showed the highest pull-out forces (5500 N). Long uncemented stems (3324 N) and anatomical cone stems (3990 N) showed similar pull-out forces.
Conclusion
All tested stems showed small relative movements. Long cemented stems show no advantages to short cemented stems in small bone defects. The use of cones or an anatomical cone stem with hybrid cementation seems to offer good stability even for larger bone defects. The use of a short cemented stem (with or without cone) may be a suitable choice with a high potential for bone preservation in total knee arthroplasty revision with respective bone defects.
Learn more here
Preliminary clinical results of coated porous tibia cones in septic and aseptic revision knee arthroplasty
Malte Ohlmeier, Christian Lausmann, Matthias Wolff, Hussein Abdelaziz, Thorsten Gehrke, Mustafa Citak
Abstract
Purpose
To analyze the first results of calcium-phosphate-coated porous tibia cones.
Methods
Patients treated with TrabecuLink®-CaP Cones were retrospectively recruited from January 2016 to December 2017. These custom-made cones were produced using titanium alloy Ti–6Al–4 V (Tilastan®) and using additive manufacturing with a special calcium-phosphate coating (HX®-coating). Clinical outcome was evaluated using Oxford Knee Score. For radiological evaluation of the implants, patients sent us outpatient taken radiographs. A minimum follow-up of one year was required. Lastly, we analyzed postoperative complications and revision rates.
Results
52 patients with revision knee arthroplasty (RKA) were recruited for final analysis, of whom, we had 17 septic RKAs (33%) and 35 aseptic cases of RKA (67%). The bone defects were grouped into 17 AORI Type 2A (32.7%), 14 Type 2B (26.9%) and 21 Type 3 (40.4%). After a mean follow-up of 22 months (13.2–34.8; SD = ± 10), we had 4 surgical revisions (7.7%), 2 septic and 2 aseptic cases. The mean Oxford Knee Score was 28.6 points (8–47; SD = ± 10). 22 of 28 radiographs (78.6%) showed regular positioning of the cones and TKAs at a mean follow-up of 16.8 months (13.2–34.8; SD = ± 6). Three patients (10.7%) showed slight radiolucencies in the bone–cement interfaces and 3 patients (10.7%) had beginning heterotopic ossifications.
Conclusions
This study shows the initial clinical results of calcium-phosphate-coated tibia cones showing a good functional outcome. Further research should focus on long-term clinical and radiological follow-up.
Learn more here
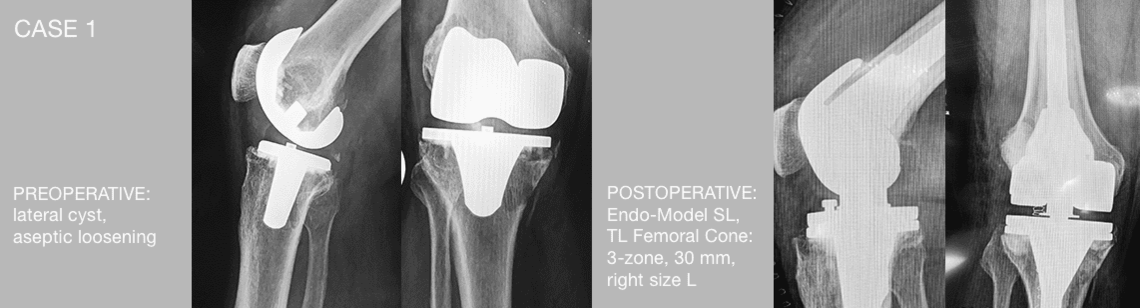
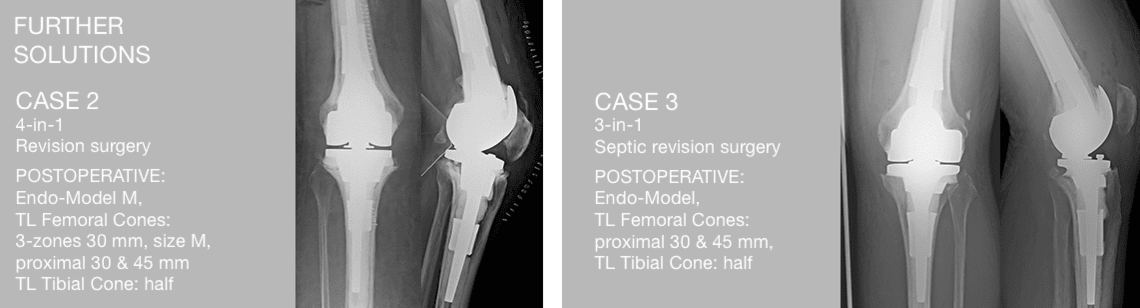
Longer Femoral Cones addresses even zone 2.5.
For more LINK product webinars visit our: Medical Education Webinar Channel
PAPER R. MORGAN-JONES
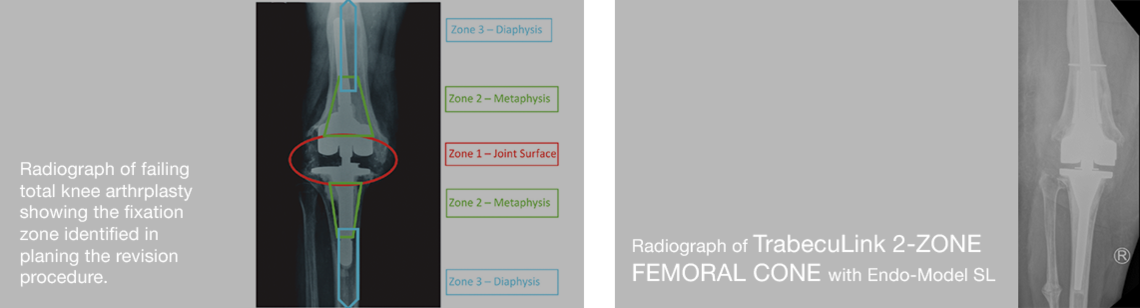
Zonal Fixation in revision total knee arthroplasty
Zonal fixation in revision total knee arthroplasty R Morgan-Jones, S I S Oussedik, H Graichen, F S Haddad Affiliations
PMID: 25628273 DOI: 10.1302/0301-620X.97B2.34144
Abstract
Revision knee arthroplasty presents a number of challenges, not least of which is obtaining solid primary fixation of implants into host bone. Three anatomical zones exist within both femur and tibia which can be used to support revision implants. These consist of the joint surface or epiphysis, the metaphysis and the diaphysis. The methods by which fixation in each zone can be obtained are discussed. The authors suggest that solid fixation should be obtained in at least two of the three zones and emphasise the importance of pre-operative planning and implant selection.
Keywords: Multi-zone strategy; Revision total knee replacement; Zonal fixation.
©2015 The British Editorial Society of Bone & Joint Surgery.
Learn more about the zonal fixation here
Use of porous custom-made cones for meta-diaphyseal bone defects reconstruction in knee revision surgery: a clinical and biomechanical analysis
Giorgio Burastero, Silvia Pianigiani, Cristiana Zanvettor, Luca Cavagnaro, Francesco Chiarlone, Bernardo Innocenti
Abstract
Introduction: Although the practice of metaphyseal reconstruction has obtained successful clinical and radiological results in revision total knee surgery, off-the-shelf devices aren't an effective solution for all patients as they do not cover the full range of clinical possibilities. For this reason, during severe knee revisions, custom-made porous titanium cementless metaphyseal cones are nowadays employed as alternative to traditional surgeries. The aim of this study is to understand the benefits gained by the use of the custom-made cones against the performance of more traditional techniques, such as the use of cemented or cementless stems. Thus, a retrospective study on eleven patients and a biomechanical finite element analysis (FEA) was developed, based upon three clinical cases of the clinical analyzed cohort.
Materials and methods: Eleven patients underwent staged total knee arthroplasty revision with the use of 16 custom-made cones to correct severe femoral and tibial meta-diaphyseal bone defects. Clinical scores and range of movement were observed during the follow-up period (mean follow-up 26 ± 9.4 months). Reason for surgery was periprosthetic joint infection (PJI) in eight patients and post-traumatic osteomyelitis in the other three patients. Three patients previously affected by PJI were selected among the eleven patients of the clinical population. For those patients, bone geometries and implants during surgery were replicated in silico and analyzed during different daily activities. For the same patients, as alternative solution for surgery, the use of cemented or cementless stems was also simulated by FEA. Stress patterns in different region of interest and risk of fracture in the bone were calculated and compared.
Results: No loosening, component migration, or mismatches between preoperative planning and intraoperative findings were clinically registered. Biomechanical results demonstrated that the use of custom-made cones induces a more homogeneously distributed bone stress than the other two techniques that concentrate the stress in spotted regions. The risk of fracture is comparable between the use of custom-made cones and cemented technique, while press-fit configurations increase the risk of fracture (more than 35%).
Conclusions: Based upon the clinical evidence and the findings after the FEAs, the practice of porous custom-made metaphyseal cones in severe revisions of knee arthroplasties is showing promising biomechanical results. The homogeneous stresses distributions and the lower bone stress gradient could justify a reduction of bone fractures and the risk of implant loosening which could be the explanation to the successful clinical outcomes.
Keywords: Bone stress; Clinical analysis; Custom-made cone; Revision TKA; Severe bone defect; Stem.
Learn more here
METAPHYSEAL CONES AND SLEEVES IN REVISION TOTAL KNEE ARTHROPLASTY: TWO SIDES OF THE SAME COIN?
Complications, clinical and radiological results—a systematic review of the literature A. Zanirato1 · M. Formica1 · L. Cavagnaro2 ·
S. Divano1 · G. Burastero2 · L. Felli1 Received: 10 December 2018 / Accepted: 8 February 2019 © Istituto Ortopedico Rizzoli
2019
Abstract
Revision total knee arthroplasty (rTKA) is increasing of relevance in orthopaedic surgeon daily practice and this trend is likely to continue in the years ahead. The aim of this systematic review of English literature is to summarize and compare indications, complications, clinical and radiological results of metaphyseal cones and sleeves in management of bone loss in rTKA. Retrospective or prospective studies with at least 1 year of follow-up (FU) were included. The PRISMA 2009 flowchart and checklist were considered to edit the review. Clinical and radiological results, rates of intraoperative fractures, aseptic loosening, periprosthetic joint infection, septic failure, reoperations and re-revisions were extrapolated by the papers. Thirty-seven articles were included in the systematic review. Results of 927 cones (mean FU of 3.6 ± 1.4 years) and 1801 sleeves (mean FU of 4.5 ± 1.6 years) were analysed. The studies showed good clinical and functional outcomes. Cones and sleeves allowed a stable metaphyseal fixation. The aseptic survivorship of the implants was 97.3% in cones group and 97.8% in sleeves group. Metaphyseal cones and sleeves represent a viable option in management f type IIb and III AORI bone defects in aseptic and septic TKAr with overlapping survival rate. Further high-quality long-term studies would better clarify complications, clinical and radiological results of these promising techniques in revision total knee arthroplasty.
Learn more here
In our experience with Link FlexiCones, most of our patient cases have involved the available sizes and variants. For even more challenging patient cases we can offer custom-made implants. We have a department that focuses on special cases. We are happy to support you and your patients. Please visit us: customlink.solutions