Rebuilding the Ankle: Custom Distal Tibial Replacement after Allograft Failure

A Custom Distal Tibial Replacement: Restoring Joint Function after Allograft Failure
Massive bone defects of the distal tibia are rare, yet they represent some of the most challenging reconstructive scenarios in
orthopedic surgery. They typically occur after trauma, infection, tumor resection, or—as in this case—after the failure of an allograft.
When conventional reconstruction strategies such as revision osteosynthesis or repeated bone grafting are not feasible, surgeons
often have limited options for restoring stability and articulation of the ankle joint. This case study demonstrates how a fully customized
solution can facilitate functional reconstruction when biological principles and standard implants are ineffective.
Preserving Motion: Resection with Function in Mind
A 75-year-old male patient weighing 100 kg presented with a history of a distal tibial fracture, which had initially been treated with allograft reconstruction.
Over time, however, the graft failed, resulting in loss of fixation, instability, and non-union. This resulted in mechanical insufficiency and functional impairment,
causing significant pain and limiting weight-bearing capacity.
The surgical objective was ambitious: to replace the distal tibia with a patient-specific implant that would restore stability
and preserve ankle joint motion by integrating an articulated talus component. At the same time, the solution had to ensure
long-term fixation without the use of cement to allow for biological integration and potential longevity.

Figure 1: (Left) Preoperative 3D reconstruction of the distal tibia, demonstrating the extensive bone loss that occurred following allograft failure. (Right) Preoperative imaging shows failed fixation, a broken nail, and non-union of the distal tibia.
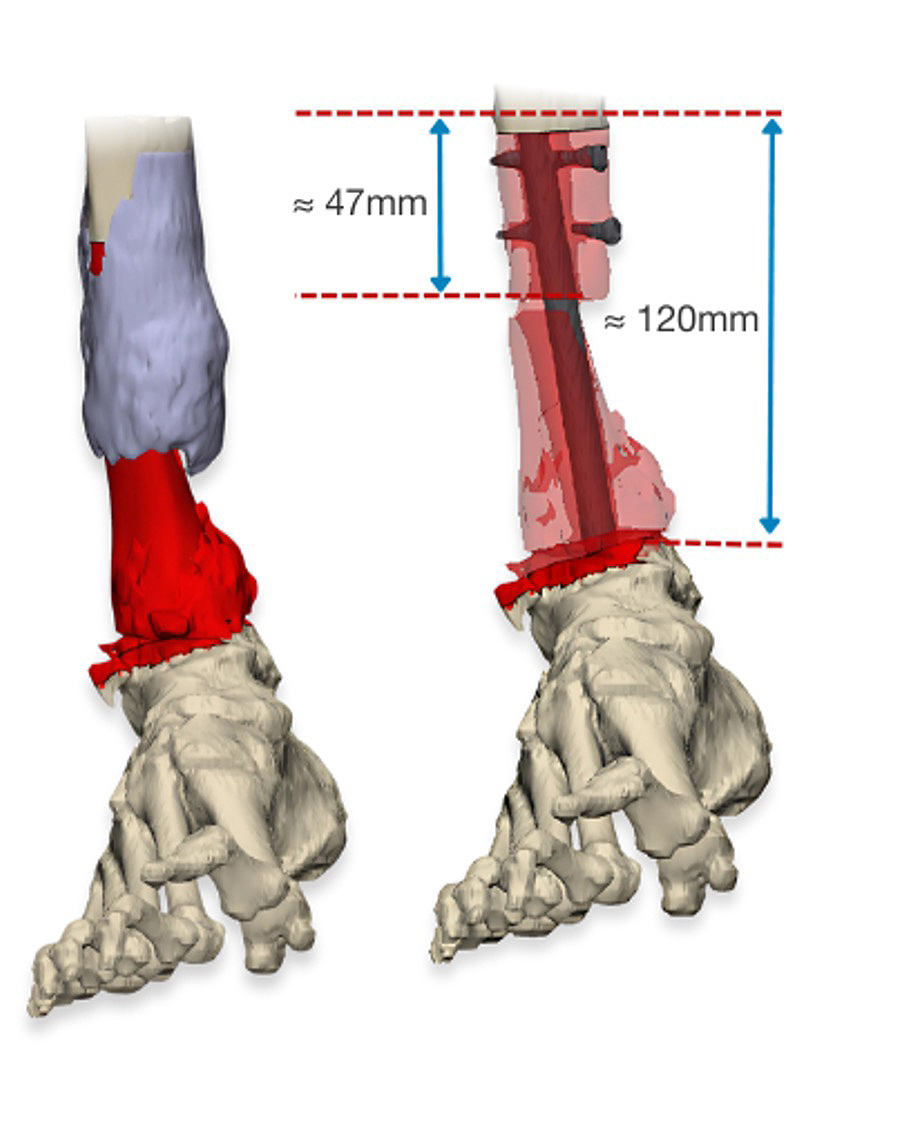
Figure 2: (Left) Virtual resection planning, showing color-coded zones that illustrate the extent of bone removal. (Right) Resection and alignment simulation for custom implant positioning.
Tailored Implant Strategy: Modularity and Osseointegration
In close collaboration with the surgical team responsible for the patient’s treatment, customLINK developed a patient-specific distal tibia replacement.
The design was based on CT data and virtual surgical planning, enabling exact matching to the patient’s anatomy and defect size. Several critical aspects
were addressed during development:
- Modular tibial replacement to allow intraoperative flexibility and adaptation to unforeseen bone conditions.
- A talus component with a PorEx® coating on the articulating surface to minimize wear, combined with a TrabecuLink® structure
on the areas that will be in contact with the bone to promote reliable osseointegration. - A cementless MEGASYSTEM-C® stem offering compatibility with standard modular components and providing
stable diaphyseal fixation. - Custom-made instruments and saw guides to ensure precise resection according to the virtual plan and accurate implant alignment.
This strategy combined mechanical stability, biological integration, and functional preservation—three essential
prerequisites for successful reconstruction in such a complex case.
This strategy combined mechanical stability, biological integration, and functional preservation—three essential
prerequisites for successful reconstruction in such a complex case.
The procedure was performed using patient-specific saw guides to facilitate reproducible bone cuts and optimal implant positioning.
After resection of the failed allograft and preparation of the host bone, the custom implant was inserted. The cementless stem achieved
immediate primary stability, and the TrabecuLink® surfaces were expected to provide accelerated osseointegration. The talus component
restored articulation with the tibial replacement, allowing preserved ankle motion. Intraoperative stability was excellent, and no technical
complications occurred. Postoperatively, the patient was mobilized with partial weight-bearing and transitioned into a structured rehabilitation
program. Early X-rays confirmed correct alignment and stable fixation.

Figure 3: (Left) The final 3D design of the custom distal tibial replacement with a talus component. (Right) Implant model showing the modular tibial replacement with TrabecuLink® structures.
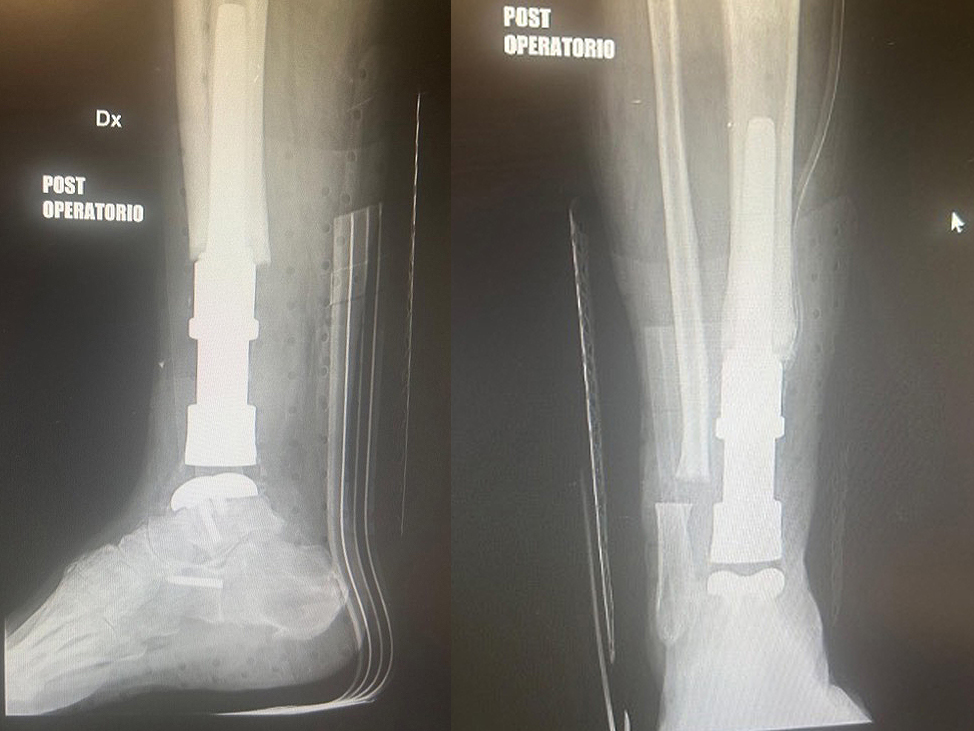
Figure 4: (Left) Postoperative X-ray (lateral view) confirming the correct positioning and cementless fixation of the custom implant. (Right) Anteroposterior view demonstrating stable alignment and restoration of articulation.
Discussion and Conclusion
Reconstruction of large distal tibial defects remains one of the most demanding challenges in limb salvage surgery. Biological solutions, such as allografts
or vascularized bone transfers, can fail due to limited healing potential, a high risk of resorption or mechanical insufficiency under load. Standard mega-prosthetic
solutions often lack the anatomical fit and functional articulation required for the ankle joint.
This case study demonstrates the importance of patient-specific implants in overcoming these limitations. Integrating modern surface technologies such as TrabecuLink®
for osseointegration, advanced coatings such as PorEx® for articulation, and modular designs for intraoperative flexibility enables custom solutions to address both
biomechanical and biological demands. Such implants not only restore structural integrity and stability but also preserve mobility and function—key factors for the patient’s
quality of life.
Clinical Implications
Careful preoperative planning, close collaboration between the surgeon and the implant developer, and the use of customized instrumentation
were all essential to the success of this case. The patient-specific distal tibial replacement enabled the restoration of joint function where conventional
approaches had failed.
This example demonstrates the potential of custom implants to enhance surgical options for complex reconstructions, facilitating early mobilization,
long-term fixation, and functional recovery.